Abstract
OBJECTIVE: To explore the role of the gender of the patient and the gender of the physician in explaining differences in patient satisfaction and patient-reported primary care practice.
DESIGN: Cross-sectional mailed survey [response rate of 71%].
SETTING: A large group-model Health Maintenance Organization (HMO) in northern California.
PATIENTS/PARTICIPANTS: Random sample of HMO members aged 35 to 85 years with a primary care physician. The respondents (N=10,205) were divided into four dyads: female patients of female doctors; male patients of female doctors; female patients of male doctors; and male patients of male doctors. Patients were also stratified on the basis of whether they had chosen their physician or had been assigned.
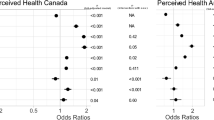
MEASUREMENTS AND MAIN RESULTS: Among patients who chose their physician, females who chose female doctors were the least satisfied of the four groups of patients for four of five measures of satisfaction. Male patients of female physicians were the most satisfied. Preventive care and health promotion practices were comparable for male and female physicians. Female patients were more likely to have chosen their physician than males, and were much more likely to have chosen female physicians. These differences were not seen among patients who had been assigned to their physicians and were not due to differences in any of the measured aspects of health values or beliefs.
CONCLUSIONS: Our study revealed differences in patient satisfaction related to the gender of the patient and of the physician. While our study cannot determine the reasons for these differences, the results suggest that patients who choose their physician may have different expectations, and the difficulty of fulfilling these expectations may present particular challenges for female physicians.
Similar content being viewed by others
References
Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women: does the sex of the physician matter? New Eng J Med. 1993;329:478–82.
Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33:407–16.
Hall JA, Palmer RH, Orav EJ, Hargraves JL, Wright EA, Louis TA. Performance quality, gender, and professional role. Med Care. 1990;28:489–501.
Battista RN, Williams JI, MacFarlane LA. Determinants of preventive practices in fee-for-service primary care. Am J Prev Med. 1990;6:6.
Levy S, Dowling P, Boult L, et al. The effect of physician and patient gender on preventive medicine practices in patients older than fifty. Fam Med. 1992;24:58–61.
Osborn EH, Bird JA, McPhee SJ, et al. Cancer screening by primary care physicians: can we explain the differences. J Fam Pract. 1991;32:465–71.
Franks P, Clancy CM. Physician gender bias in clinic decision-making: screening for cancer in primary care. Med Care. 1993;31:213–8.
Roter D, Lipkin M Jr, Korsgaard A. Sex differences in patients’ and physicians’ communication during primary care medical visits. Med Care. 1991;29:1083–93.
Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Satisfaction, gender, and communication in medical visits. Med Care. 1994;32:1216–31.
Elderkin-Thompson V, Waitzkin H. Differences in clinical communication by gender. J Gen Intern Med. 1999;14:112–21.
Meeuwesen L, Schaap C, van der Staak C. Verbal analysis of doctor-patient communication. Soc Sci Med. 1991;32:1143–50.
Roter DL, Hall JA. Why physician gender matters in shaping the physician-patient relationship. J Womens Health. 1998;7:1093–7.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9.
Linn LS, Cope DW, Leake B. The effect of gender and training of residents on satisfaction ratings by patients. J Med Educ. 1984;59:964–6.
Bertakis K, Robbins J. Gatekeeping in primary care: a comparison of internal medicine and family practice. J Fam Pract. 1987;24:305–9.
Wallen J, Waitzkin H, Stoeckle J. Physician stereotypes about female health and illness: a study of patients’ sex and the informative process during medical interviews. Women Health. 1979;4:135–46.
Verbrugge L. Sex differences in complaints and diagnosis. J Behav Med. 1980;3:327–55.
Nathanson C. Illness and feminine role: a theoretical review. Soc Sci Med. 1975;9:57–63.
Hall J, Roter D. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;26:651–9.
Waitzkin H. Information giving in medical care. J Health Soc Behav. 1985;26:81–101.
Waitzkin H. Doctor-patient communication. JAMA. 1984;252:2441–6.
Kravitz RL, Greenfield S, Rogers W, Manning W Jr, Zubkoff M, Nelson EC. Differences in the mix of patients among medical specialties and systems of care. JAMA. 1992;267:1617–23.
Zuger A. What doctors of both sexes think of patients of both sexes. New York Times. June 21, 1998.
Steinhauer J. For women in medicine, a road to compromise, not perks. New York Times Online. March 1, 1999.
Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74:171.
Schmittdiel J, Selby JV, Grumbach K, Quesenberry CP. Choice of a personal physician and patient satisfaction in a health maintenance organization. JAMA. 1997;278:1596–9.
Grumbach K, Selby JV, Schmittdiel J, Quesenberry CP. Quality of primary care according to physician specialty. Health Serv Res. 1999;34:485–502.
Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney C, Ware JE. Patients’ ratings of outpatient visits in different practice settings: results from the Medical Outcomes Study. JAMA. 1993;270:835–40.
McBride C, Shugars D, DiMatteo R, Lepper H, O’Neil E, Damush T. The physician’s role: views of the public and the profession on seven aspects of patient care. Arch Fam Med. 1994;3:948–53.
Brown R, Hill J. The effect of Medicare risk HMOs on Medicare costs and service utilization. In: Luft H, ed. HMOs and the Elderly. Ann Arbor, Mich: Health Administration Press; 1994:13–45.
Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, Mass: The Health Institute, New England Medical Center; 1995.
Liang K-Y, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22.
McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K for the JGIM Career Satisfaction Study Group. The work lives of women physicians: results from the Physician Work Life Study. J Gen Intern Med. 2000;15:372–80.
Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Gender in medical encounters: an analysis of physician and patient communication in a primary care setting. Health Psychol. 1994;13:384–92.
Greenfield S, Nelson EC, Zubkoff M, et al. Variations in resource utilization among medical specialties and systems of care. Results from the Medical Outcomes Study. JAMA. 1992;267:1624–30.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research is supported by grant RO1-HS08269 from the Agency for Health Care Policy and Research. The authors wish to acknowledge the invaluable contributions of our project coordinator, Alison F. Truman, MS.
Rights and permissions
About this article
Cite this article
Schmittdiel, J., Grumbach, K., Selby, J.V. et al. Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J GEN INTERN MED 15, 761–769 (2000). https://doi.org/10.1046/j.1525-1497.2000.91156.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2000.91156.x