Abstract
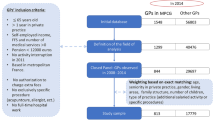
Most western countries employ a combination of fee-for-service, fixed salary and per capita subsidies to finance the services of general practitioners. Based on Norwegian data, the authors demonstrate that these fianancial schemes have been used in different types of municipalities.
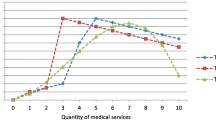
The authors argue that the fee-for-service and per capita components should be allowed to vary between primary physicians and municipalities: (a) If the patient population per primary physician is low and patient supply is unstable, the per capita subsidy or work-free income should be differentiated to ensure recruitment of physicians. (b) Physicians in municipalities with low physician coverage should be allotted a low basic grant, whilst per capita subsidy and fee-for-service payments should be used to stimulate service production. The opposite situation exists where there is a potential of supplier inducement due to high physician coverage. (c) The responsibility for designing contracts should be assigned to local rather than national authorities.
These suggestions go against important elements in the reform of primary physician services in Norway.
Similar content being viewed by others
References
R.J. Arnould, R.F. Rich and W.D. White, Competitive Approaches to Health Care Reform (The Urban Institute Press, Washington DC, 1993).
Å. Blomqvist, The doctor as double agent: information asymmetry, health insurance, and medical care, Journal of Health Economics 10(4) (1991) 411–432.
R.P. Ellis and T.G. McGuire, Optimal payment systems for health services, Journal of Health Economics 9 (1990) 375–396.
R. Evans, Supplier-induced demand: some empirical evidence and implications, in: The Economics of Health and Medical Care, ed. M. Perlman (Macmillan, Edinburgh, 1974).
J.E. Finnvold, Kan misfornøyde pasienter gi oss bedre helsetjenester, Samfunnsspeilet 3 (1998) 16–27.
H.E. Frech, ed., Regulating Doctors' Fees: Competition, Benefits, and Controls under Medicare (The AEI Press, Washington DC, 1991).
A. Krasnik, P.P. Groenewegen, P.A. Pedersen, P.V. Scholten, G. Mooney, A. Gottschau, H.A. Flierman and M.T. Damsgaard, Changing remuneration systems: Effects on activity in general practice, British Medical Journal 300 (1990) 1698–1706.
I. Lerang, Helse-og sosialsjefene: Vurdering av legetjenesten, kontraktsforhold og fastlegeordningen, Handelshøyskolen BI (1999).
Ministry of Health and Social Affairs, Innstilling fra sosialkomiteen om legetjenesten i kommunene og fastlegeordningen [Trygghet og ansvarlighet], Innst. S. nr. 215 [1996–97], Oslo (1997).
Ministry of Health and Social Affairs, Prosjektplan Fastlegeordningen, Oslo (1998).
J.P. Newhouse, W.G. Manning, E.B. Keeler and E.M. Sloss, Adjusting capitation rates using objective health measures and prior utilization, Health Care Financing Review 10(3) (1989) 41–54.
J.P. Newhouse, Pricing and imperfections in the medical care marketplace, in: Health Economics Worldwide, eds. P. Zweifel and H.E. Frech (Kluwer Academic, The Netherlands, 1992).
J.P. Newhouse, Reimbursing health plans and health providers: efficiency in production versus selection, Journal of Economic Literature 34 (1996) 1236–1263.
J.P. Newhouse, Rate adjusters for Medicare under capitation, Health Care Review (annual suppl.) (1996) 45–55.
G.C. Pope and T.B. Burge, Inefficiencies in physician practices, Advances in Health Economics and Health Services Research 13 (1992) 129–164.
T.H. Rice and R.J. Labelle, Do physicians induce demand for medical services?, Journal of Health Politics, Policy and Law 14 (1989) 587–600.
T.M. Selden, A model of capitation, Journal of Health Economics 9 (1990) 397–409.
Statistics Norway, Statistical Yearbook 1995 (Oslo/Kongsvinger, 1995).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sørensen, R.J., Grytten, J. Contract design for primary care physicians: Physician location and practice behaviour in small communities. Health Care Management Science 3, 151–157 (2000). https://doi.org/10.1023/A:1019041307532
Issue Date:
DOI: https://doi.org/10.1023/A:1019041307532