Abstract
Background
Advance directives promise to preserve patient autonomy, but research indicates that end-of-life preferences can be influenced by the way in which questions are posed.
Objective
To determine whether preferences expressed by geriatric patients on advance directives are influenced by the default response inherent in the question.
Design
Mailed survey containing 1 of 3 versions of an advance directive.
Setting
General internal medicine outpatient medical practice.
Participants
Outpatients aged 65 or older (n = 106, response rate = 27%).
Interventions
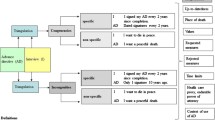
In the “withhold” version of the survey, participants indicated situations where they would want treatments withheld (i.e., the default preference was in favor of treatment). In the “provide” version, participants indicated situations where they would want treatment provided (i.e., the default preference was against treatment). In the forced-choice control version, participants made an explicit decision to withhold or provide treatment for each situation.
Main Outcome Measure
Participants’ treatment preferences.
Results
Preferences differed by condition, F(2, 103) = 3.61, MSE = 0.09, η 2 = .07, p = .03. Participants tended to express the default preference, and thus, were more likely to favor treatment in the “withhold” condition than in the “provide” condition. Preferences in the forced-choice control condition were intermediate.
Conclusions
The default inherent in a question can impact preferences for medical treatment. This default effect limits the utility of advance directives.
Similar content being viewed by others
References
Ditto PH, Hawkins NA. Advance directives and cancer decision making near the end of life. Health Psychol. 2005;24(4):S63–S70.
Fagerlin A, Schneider CE. Enough: the failure of the living will. Hastings Cent Rep. 2004;34(2):30–42.
Ditto PH, Danks JH, Smucker WD, et al. Advance directives as acts of communication. Arch Intern Med. 2001;161(3):421–30.
Coppola KM, Ditto PH, Danks JH, et al. Accuracy of primary care and hospital-based physicians’ predictions of elderly outpatients’ treatment preferences with and without advance directives. Arch Intern Med. 2001;161(3):431–40.
Johnson EJ, Goldstein D. Do defaults save lives? Science. 2003;302(5649):1338–9.
Johnson EJ, Steffel M, Goldstein D. Making better decisions: from measuring to constructing preferences. Health Psychol. 2005;24(4):S17–S22.
Redelmeier DA, Shafir E. Medical decision making in situations that offer multiple alternatives. JAMA. 1995;273(4):302–5.
Payne JW, Bettman JR, Johnson EJ. The Adaptive Decision Maker. New York, NY: Cambridge University Press; 1993.
Kressel LM, Chapman GB. Default effects in end of life treatment preferences. Med Decis Making. In press.
Madrian BC, Shea DF. The power of suggestion: Inertia in 401(k) participation and savings behavior. Q J Econ. 2001;116(4):1149–525.
Schweitzer M. Disentangling status quo and omission effects: an experimental analysis. Org Behav Human Decis Process. 1994;58:457–76.
McKenzie CR, Liersch MJ, Finkelstein SR. Recommendations implicit in policy defaults. Psychol Sci. 2006;17(5):414–20.
Acknowledgments
This research was supported by NSF award SES-03-25080 to the second author. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. A preliminary report of these results appeared as a poster presentation at the November 2006 annual meeting of the Society for Judgment and Decision Making in Houston, TX.
Conflicts of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kressel, L.M., Chapman, G.B. & Leventhal, E. The Influence of Default Options on the Expression of End-of-Life Treatment Preferences in Advance Directives. J GEN INTERN MED 22, 1007–1010 (2007). https://doi.org/10.1007/s11606-007-0204-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0204-6