Abstract
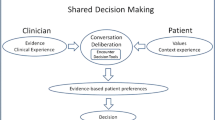
In patient centred care, shared decision making is a central feature and widely referred to as a norm for patient centred medical consultation. However, it is far from clear how to distinguish SDM from standard models and ideals for medical decision making, such as paternalism and patient choice, and e.g., whether paternalism and patient choice can involve a greater degree of the sort of sharing involved in SDM and still retain their essential features. In the article, different versions of SDM are explored, versions compatible with paternalism and patient choice as well as versions that go beyond these traditional decision making models. Whenever SDM is discussed or introduced it is of importance to be clear over which of these different versions are being pursued, since they connect to basic values and ideals of health care in different ways. It is further argued that we have reason to pursue versions of SDM involving, what is called, a high level dynamics in medical decision-making. This leaves four alternative models to choose between depending on how we balance between the values of patient best interest, patient autonomy, and an effective decision in terms of patient compliance or adherence: Shared Rational Deliberative Patient Choice, Shared Rational Deliberative Paternalism, Shared Rational Deliberative Joint Decision, and Professionally Driven Best Interest Compromise. In relation to these models it is argued that we ideally should use the Shared Rational Deliberative Joint Decision model. However, when the patient and professional fail to reach consensus we will have reason to pursue the Professionally Driven Best Interest Compromise model since this will best harmonise between the different values at stake: patient best interest, patient autonomy, patient adherence and a continued care relationship.
Similar content being viewed by others
Notes
Since Emanuel and Emanuel [8] criticises the patient choice model (which they call the informative model) for its lack of caring ingredients, it appears that they believe the venting, affirmation and caring models of sharing to be better suited to paternalism. Possibly, this may be due to a confusion of the (true) fact that all of these models of sharing connect to beneficence (which may conflict with autonomy) with the (false) assumption that beneficence can never be combined with a concern for autonomy. There is, as they note, a possibility of the professional to some extent influencing the decision of the patient by showing an interest and/or attending to his emotional needs. However, this in itself does not make for any paternalism—as long as the professional does not exploit these needs of the patient in order to covertly assume control over the decision making process.
Emanuel and Emanuel [8] see this as strength of the interpretative model over patient choice. As will transpire, however, this aspect may perfectly well be incorporated in the patient choice model.
Sandman L. The Concept of Negotiation in Shared Decision Making, Health Care Analysis, accepted.
References
Beauchamp, T. L., & Childress, J. F. (2001). Principles of biomedical ethics. New York: Oxford University Press.
Brock, D. W., & Wartman, S. A. (1990). When competent patients make irrational choices. New England Journal of Medicine, 322(22), 1595–1599.
Charles, C., Gafni, A., & Whelan, T. (1997). Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Social Science and Medicine, 44(5), 681–692.
Charles, C., Gafni, A., & Whelan, T. (1999). Decision-making in the physician–patient encounter: Revisiting the shared decision-making model. Social Science and Medicine, 49, 651–661.
CIOMS. (2002). International ethical guidelines for biomedical research involving human subjects. Geneva: CIOMS.
Deetz, S. A. (1992). Democracy in an age of corporate colonization: Developments in communication and the politics of everyday life. Albany: State University of New York.
Eddy, D. M. (1990). Anatomy of a decision. Journal of the American Medical Association, 263, 441.
Emanuel, E. J., & Emanuel, L. L. (1992). Four models of the physician-patient relationship. Journal of the American Medical Association, 267(16), 2221–2226.
Evans, R. G. (1984). Strained mercy: The economics of canadian health care. Toronto: Butterworths.
Faden, R. R., & Beauchamp, T. L. (1986). A history and theory of informed consent. New York: Oxford University Press.
Forester, J. (1989). Planning in the faces of power. Berkeley: University of California Press.
Habermas, J. (1979). Communication and evolution of society. Boston: Beacon Press.
Haywood, K., Marschall, S., & Fitzpatrick, R. (2006). Patient participation in the consultation process. A structured review of intervention strategies. Patient Education and Counseling, 63, 12–23.
Juth, N. (2005). Genetic information. Values and rights. The morality of presymptomatic genetic testing. Göteborg: Acta Universitatis Gothoburgensis.
Kettner, M. (1993). Scientific knowledge, discourse ethics, and consensual formation in the public domain. In R. Winkler & J. Cooms (Eds.), Applied ethics: A reader (pp. 28–46). Oxford: Blackwell.
Kiesler, D. J., & Auerbach, S. M. (2006). Optimal matches of patient preferences for information, decision-making and intepersonal behaviour: Evidence, models and interventions. Patient Education and Counseling, 61, 319–341.
Lewin, S. A., Skea, Z. C., Entwistle, V., Zwarenstein, M., & Dick, J. (2001). Interventions for providers to promote a patient-centred approach in clinical consultations (Review). Cochrane Database of Systematic Reviews (4), CD003267.
Lutfey, K. E., & Wishner, W. J. (1999). Beyond “Compliance” Is “Adherence”. Improving the prospect of diabetes care. Diabetes Care, 22(4), 635–639.
Makoul, G., & Clayman, M. L. (2006). An integrative model of shared decision making in medical encounters. Patient Education and Counseling, 60, 301–312.
Munthe, C. (1999). Pure selection: The ethics of preimplantation genetic diagnosis and choosing children without abortion. Göteborg: Acta Universitatis Gothoburgensis.
Provis, C. (2004). Negotiation, persuasion and argument. Argumentation, 18, 95–112.
Rao, J. K., Anderson, L. A., Inui, T. S., & Frankel, R. M. (2007). Communication interventions make a difference in conversations between physicians and patients. Medical Care, 45(4), 340–349.
Savulescu, J. (1995). Rational non-interventional paternalism: Why doctors ought to make judgments of what is best for their patients. Journal of Medical Ethics, 21(6), 327–331.
Savulescu, J., & Momeyer, R. W. (1997). Should informed consent be based on rational beliefs? Journal of Medical Ethics, 123(5), 282–288.
Sycara, K. P. (1990). Persuasive argumentation in negotiation. Theory and Decision, 28, 203–242.
van Dam, H. A., van der Horst, F., van den Borne, B., Ryckman, R., & Crebolder, H. (2003). Provider-patient interaction in diabetes care: Effects on patient self-care and outcomes. A systematic review. Patient Education and Counseling, 51, 17–28.
VanDeVeer, D. (1992). Paternalistic intervention. The moral bounds on belevolence. Princeton: Princeton University Press.
Wirtz, V., Cribb, A., & Barber, N. (2006). Patient-doctor decision-making about treatment within the consultation—a critical analysis of models. Social Science and Medicine, 62(1), 116–124.
World Medical Association. (2004) World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. WMA.
Acknowledgments
The article is written within PICAP, a project to implement patient centred care for patients with chronic heart failure. The project is financed by Gothenburg University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sandman, L., Munthe, C. Shared Decision Making, Paternalism and Patient Choice. Health Care Anal 18, 60–84 (2010). https://doi.org/10.1007/s10728-008-0108-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10728-008-0108-6