Abstract
Purpose
To examine the attitudes and preferences of surrogate decision makers (SDMs) regarding their involvement in the consent to research process for ICU patients.
Methods
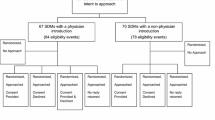
We presented 136 SDMs of critically ill patients in five ICUs with four hypothetical research scenarios: baseline interventional study of a placebo controlled RCT; study with higher risk of treatment complication; study comparing two accepted treatments; study with shorter enrolment window. For each we asked SDMs if they would want to be involved in the consent to research decision, and to rate the acceptability of their comfort with, and their sense of burden with their involvement. Participants were screened for symptoms of anxiety and depression using the Hospital Anxiety and Depression Scale.
Results
For the baseline scenario, most SDMs wished to be involved in research decision making (90 %; 95 % CI 84–95 %); responses varied little across study permutations. The majority considered their involvement to be acceptable (85 %; 95 % CI 77–90 %), whereas, a small minority rated it as being unacceptable (2 %; 95 % CI 1–6 %). Many were comfortable with being involved (50 %; 95 % CI 41–59 %), but the number decreased when risk of harm was higher (34 %; 95 % CI 26–43 %) or enrolment window was shorter (41 %; 95 % CI 33–50 %). A majority (62 %) reported symptoms of anxiety and many (38 %) had symptoms of depression.
Conclusion
Most of the interviewed SDMs wished to be involved in research decision making for critically ill and incapable loved ones. Variability existed, however, in their desire to be involved when decisions were time-sensitive or perceived risk was greater.





Similar content being viewed by others
References
Luce JM, Cook DJ, Martin TR, Angus DC, Boushey HA, Curtis JR, Heffner JE, Lanken PN, Levy MM, Polite PY, Rocker GM, Truog RD, American Thoracic Society (2004) The ethical conduct of clinical research involving critically ill patients in the United States and Canada: principles and recommendations. Am J Respir Crit Care Med 170:1375–1384
Fan E, Shahid S, Kondreddi VP, Bienvenu OJ, Mendez-Tellez PA, Pronovost PJ, Needham DM (2008) Informed consent in the critically ill: a two-step approach incorporating delirium screening. Crit Care Med 36(1):94–99
Scales DC, Smith OM, Pinto R, Barrett KA, Friedrich JO, Lazar NM, Cook DJ, Ferguson ND (2009) Patient’s preferences for enrolment into critical-care trials. Intensive Care Med 35:1703–1712
Lazar NM, Greiner GG, Robertson G, Singer PA (1996) Bioethics for clinicians. 5. Surrogate decision-making. CMAJ 155:1435–1437
Buchanan AE, Brock DW (1989) Deciding for others. Cambridge University Press, Cambridge
Beauchamp TL, Childress JF (2001) Principles of biomedical ethics. Oxford University Press, USA
Anonymous(2007)Directive 2001/20/EC of the European Parliament and of the Council of 4 April 2001 on the approximation of the laws, regulations and administrative provisions of the member states relating to the implementation of good clinical practice in the conduct of clinical trials on medicinal products for human use. Off J Eur Commun1:33–44
Chenaud C, Merlani P, Verdon M, Ricou B (2009) Who should consent for research in adult intensive care? Preferences of patients and their relatives: a pilot study. J Med Ethics 35:709–712
Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, le Gall JR, Dhainaut JF, Schlemmer B; French FAMIREA Group (2001) Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 29:1893–1897
Myhren H, Ekeberg I, Langen I, Stokland O (2004) Emotional strain, communication, and satisfaction of family members in the intensive care unit compared with expectations of the medical staff: experiences from a Norwegian University Hospital. Intensive Care Med 30:1–8
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larché J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B; FAMIREA Study Group (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994
McAdam JL, Dracup KA, White DB, Fontaine DK, Puntillo KA (2010) Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med 38:1078–1085
Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, Zahar JR, Schlemmer B, Azoulay E; French FAMIREA study group (2005) Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care 20:90–96
McAdam JL, Puntillo K (2009) Symptoms experienced by family members of patients in intensive care units. Am J Crit Care 18:200–209 Quiz 210
Etchells E, Darzins P, Silberfeld M, Singer PA, McKenny J, Naglie G, Katz M, Guyatt GH, Molloy DW, Strang D (1999) Assessment of patient capacity to consent to treatment. J Gen Intern Med 14:27–34
Zigmond A, Snaith R (1987) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Perner A, Ibsen M, Bonde J (2010) Attitudes to drug trials among relatives of unconscious intensive care patients. BMC Anesthesiol 10:6
Luce JM (2009) Informed consent for clinical research involving patients with chest disease in the United States. Chest 135:1061–1068
Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Peters S, Tranmer JE, O’Callaghan CJ (2003) Decision-making in the ICU: perspectives of the surrogate decision-maker. Intensive Care Med 29:75–82
Azoulay E, Pochard F, Chevret S, Adrie C, Annane D, Bleichner G, Bornstain C, Bouffard Y, Cohen Y, Feissel M, Goldgran-Toledano D, Guitton C, Hayon J, Iglesias E, Joly LM, Jourdain M, Laplace C, Lebert C, Pingat J, Poisson C, Renault A, Sanchez O, Selcer D, Timsit JF, Le Gall JR, Schlemmer B; FAMIREA Study Group (2004) Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units*. Crit Care Med 32:1832–1838
Mehta S, Quittnat-Pelletier F, Brown M, Ethier C, Wells D, Burry L, MacDonald R (2012) Why surrogate decision makers provide or decline consent for ICU research studies: a questionnaire study. Intensive Care Med 38:47–54
Menon K, Ward RE, Gaboury I, Thomas M, Joffe A, Burns K, Cook D (2012) Factors affecting consent in pediatric critical care research. Intensive Care Med 38:153–159
Ciroldi M, Cariou A, Adrie C, Annane D, Castelain V, Cohen Y, Delahaye A, Joly LM, Galliot R, Garrouste-Orgeas M, Papazian L, Michel F, Barnes NK, Schlemmer B, Pochard F, Azoulay E; Famirea study group (2007) Ability of family members to predict patient’s consent to critical care research. Intensive Care Med 33:807–813
Acknowledgments
We thank Amardeep Bali, Mardi Baum, Joel Elman, and Stephanie Go for their help with screening of patients and data collection. Damon Scales and Ruxandra Pinto had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of interest
Drs. Ferguson and Scales are supported by New Investigator Awards, Dr. Friedrich by a Clinician Scientist Award, and Ms. Smith by a Doctoral Research Award from the Canadian Institutes of Health Research (CIHR) (Ottawa, Canada). Dr. Cook is a Canada Research Chair of the CIHR.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Barrett, K.A., Ferguson, N.D., Athaide, V. et al. Surrogate decision makers’ attitudes towards research decision making for critically ill patients. Intensive Care Med 38, 1616–1623 (2012). https://doi.org/10.1007/s00134-012-2625-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2625-x