Abstract
Objective
To determine the influence of religious affiliation and culture on end-of-life decisions in European intensive care units (ICUs).
Design and setting
A prospective, observational study of European ICUs was performed on consecutive patients with any limitation of therapy. Prospectively defined end-of-life practices in 37 ICUs in 17 European countries studied from 1 January 1999 to 30 June 2000 were compared for frequencies, patterns, timing, and communication by religious affiliation of physicians and patients and regions.
Results
Of the 31,417 patients 3,086 had limitations. Withholding occurred more often than withdrawing if the physician was Jewish (81%), Greek Orthodox (78%), or Moslem (63%). Withdrawing occurred more often for physicians who were Catholic (53%), Protestant (49%), or had no religious affiliation (47%). End-of-life decisions differed for physicians between regions and who had any religious affiliation vs. no religious affiliation in all three geographical regions. Median time from ICU admission to first limitation of therapy was 3.2 days but varied by religious affiliation; from 1.6 days for Protestant to 7.6 days for Greek Orthodox physicians. Median times from limitations to death also varied by physician's religious affiliation. Decisions were discussed with the families more often if the physician was Protestant (80%), Catholic (70%), had no religious affiliation (66%) or was Jewish (63%).
Conclusions
Significant differences associated with religious affiliation and culture were observed for the type of end of life decision, the times to therapy limitation and death, and discussion of decisions with patient families.
Similar content being viewed by others
Introduction
As each religion has its own rituals and beliefs at the end-of-life (EOL), EOL decisions vary with the physician's religious affiliation [1, 2] but other factors including country and geographical region [1, 3–11], culture [12, 13], and the physician's personal characteristics [3, 14] account for the wide variation in EOL care. The impact of such parameters on physician practice is most striking in studies of acculturation, showing that physicians' attitudes and actions are altered by exposure to a different culture [12, 13]. An understanding of the factors that affect EOL decisions in intensive care units (ICUs) throughout the world, however, remains elusive [3, 15].
Clarification of the role of religious affiliation, religiosity, tradition and culture [3, 9, 14, 15] can lead to improved physician-patient communication. European physicians tend to be more paternalistic than their North American colleagues [1, 3, 4, 16, 17]. In North America and Europe physicians are often unaware of their patients' wishes [9], or the treatment differs from what patients desire [8, 18]. In particular, physicians are not sufficiently aware of the role played by religion in their patients' preferences at the EOL. “Being at peace with God” and praying were considered more important by dying patients than physicians and “being at peace with God” and pain control were nearly identical in importance for patients [19].
The present report is the first prospective observational study evaluating religious affiliation and culture as factors in actual adult EOL practices in European ICUs; previously, religious influence has been evaluated only in questionnaires with hypothetical situations [1, 5, 6, 20]. This study [21] supplements the previous Ethicus report [3], which only briefly evaluated religious affiliation.
Methods
Study population
All consecutive adult patients admitted to the ICUs of participating centers who died or had any limitation of life-saving interventions in the ICU between 1 January 1999 and 30 June 2000 were studied prospectively. During the study 31,417 patients were admitted to ICUs in 37 centers located in 17 countries [3]. Of these patients 4,248 died or had limitations of life-sustaining treatments, and the 3,086 with EOL decisions [excluding patients with brain death and failed cardiopulmonary resuscitation (CPR)] comprised the study population. Patient characteristics are shown in Table 1, and Table 2 summarizes the religious affiliation of physicians and patients. Patients were followed until ICU discharge or death.
Definitions
EOL categories were defined prospectively as CPR, brain death, withholding life-sustaining treatment (WH), withdrawing life-sustaining treatment (WD), and active shortening of the dying process (SDP) as previously reported [3]. Active SDP was defined as a circumstance in which someone performed an act with the specific intent of shortening the dying process. Culture was defined as the habits of a given people and evaluated by the geographical region.
Ethical and legal considerations
No interventions or treatments were given, withheld, or withdrawn from patients as part of this observational study. Countries and centers were coded and study patients were numbered consecutively to ensure anonymity and confidentiality and to allow clinicians to report practices of questionable legality. Individual institutional ethics committee approval with a waiver of informed consent was required and obtained from each participating institution.
Study centers and data collection
Study data included patient and institutional characteristics. Patient characteristics were gender, age, religious affiliation, ICU admission diagnosis, chronic disorders, type of EOL category, and dates and times of ICU admission, death or discharge and decisions to limit therapy. Institutional data included country, hospital mortality rate, physician religion, practice (academic, nonacademic) and turnover [mean number of ICU admissions per month: small (up to 30), intermediate (31–60), or large (> 61)]. As physicians were anonymous, the same physician could make a decision for more than one patient. Physician numbers are for the number of patients that physicians of that religious affiliation made decisions. Countries were divided into three geographic regions prior to data analysis: Northern (Denmark, Finland, Ireland, The Netherlands, Sweden, and United Kingdom), Central (Austria, Belgium, Czech Republic, Germany, and Switzerland), and Southern (Greece, Israel, Italy, Portugal, Spain, and Turkey) [3].
Statistical analyses
Associations of categorical variables with religious affiliation were tested by the χ2 test. Time from ICU admission to first limitation of therapy and time from first limitation of therapy to death showed a marked asymmetry. Therefore the nonparametric Kruskal–Wallis analysis of variance was applied for comparisons of those “times to” between the religious affiliations. A multiple logistic regression was used to examine and test the associations of the odds for treatment limitations of withdrawing (including SDP) vs. withholding therapies with the factors age, gender, diagnosis, chronic disorder, ICU length of stay, religious affiliation, practice and turnover. Collinearity of religious affiliation and region prevented the inclusion of both variables in the model. Differences at the level of p < 0.05 were considered statistically significant; all p-values reported are two-tailed.
Results
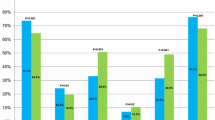
EOL decisions varied greatly depending on the physician's religious affiliation (Fig. 1). Life-sustaining treatment was withheld more often than withdrawn if the physician was Jewish, Greek Orthodox, or Moslem; if physicians had no religious affiliation or were Protestant the ratio of WH/WD was about 1 (Table 2). Catholic physicians withdrew more often than they withheld treatment. SDP occurred only if the physician was Catholic, Protestant or had no religious affiliation (Table 2), p < 0.001. Ventilators were withdrawn less frequently for Jewish, Moslem, and Greek Orthodox physicians (15/761, 2%) than for physicians of other or no religious affiliation (308/3,420, 9%, p < 0.001). As indicated in Table 2, the distribution of EOL practices associated with patients' religious affiliations was similar to practices associated with physicians' religious affiliation. The prevalence of CPR or limitations was similar in the North and Central regions regardless of whether the religious affiliation of the physician and the patient were the same. In the South, however, there was more CPR (53%) and fewer limitations (47%) if the religious affiliation of the physician and the patient were different than the same (29% and 71%, respectively, p < 0.001). An assessment of differences between regions by religious affiliation could be made only for Catholic, Protestant, and Jewish physicians as other religious affiliations were confined to a single region. No noticeable differences were found for Catholics and Protestants. Withdrawing was performed more often by Jewish physicians in the Northern (36%) than the Southern (6%) region. Physician religious affiliations by region are demonstrated in Table 3.
To evaluate the contributions and different affects of both religious affiliation and culture to EOL decisions, decisions were studied in each region for those physicians with religious affiliations or none. Figure 1 demonstrates that cultural factors are important with differences in the totals for CPR, withholding or withdrawing/SDP in the three regions. Despite these differences there are also differences within the regions associated with the presence or absence of religious affiliation. Median time from admission to ICU to first limitation of therapy varied by physician religious affiliation. It ranged from a median of 1.6 days when the physician was Protestant to a median of 7.6 days when the physician was Greek Orthodox (p < 0.001; Table 4). The time from admission to first limitation was similar for patient and physician religious affiliations. Median time from withholding therapy to death ranged from a median of 0.3 d when the physician was Jewish to 1.0 d when the physician had no religious affiliation (p < 0.001; Table 5). Median time from withdrawing therapy to death ranged from a median of 0.4 d when the physician was Protestant to 2.0 d when the physician was Jewish (p < 0.001; Table 5).
Of the 3,086 patients only 6% were mentally competent at the time of EOL decisions. Information about the patient's wishes was available for only 808 (26%) patients. Information was obtained more often when the physician was Protestant 244 (32%), had no religious affiliation 217 (32%), was Greek Orthodox 50 (30%) or Jewish 86 (28%) than if the physician were Catholic 198 (18%) or Moslem 2 (8%, p < 0.001). Of the 3,086 decisions to limit therapy in the case of 2,107 (68%) patients the decision was discussed with the patient's family. Discussions took place more often if the physician was Protestant 617 (80%), Catholic 768 (70%), had no religious affiliation 441 (66%) or was Jewish 195 (63%) than if he/she was Greek Orthodox 55 (33%), or Moslem 6 (25%, p < 0.001; Fig. 2).
Discussions by ICU physicians occurred with the primary care physicians 62% of the time and with ICU nurses 78% of the time. These discussions occurred more often if the ICU physician was Moslem, Protestant, Jewish or had no religious affiliation and less if they were Catholic or Greek Orthodox (p < 0.0001; Fig. 2). Among 979 patients for whom the EOL decision was not discussed with the family the reasons were stated in 915 cases (93%); in 405 cases (41%) because the patient was unresponsive to maximum therapy, for 230 (24%) patients, the family would not understand, and for 280 (29%) the family was unavailable. There were differences in the reasons for lack of discussions by religious affiliation. “Lack of patient responsiveness to therapy” was more commonly cited if the physician was Greek Orthodox (76%), Moslem (56%), or Catholic (47%), and less commonly if the physician was Jewish (42%), Protestant (31%), or had no religious affiliation (30%).
Multivariate analyses revealed more withdrawing (including SDP) than withholding therapies as days in ICU increased and for Catholic physicians and less withdrawing for Jewish and Greek Orthodox physicians and ICUs with small patient turnover (Table 6).
Discussion
EOL treatment involves ethical dilemmas, and under identical clinical circumstances physicians with different religious, cultural and ethical backgrounds may adopt different approaches [1–3]. Even within the same religionmajor diversities are seen as in Christianity with its Roman Catholic, Greek Orthodox, and Protestant churches [22]. This study demonstrated that EOL decisions in European ICUs vary greatly depending on regional cultural differences. Significant differences based on physician religious affiliation were also observed in the choice of EOL practices, time to therapy limitation, time from limitation to death, the availability of patient's wishes, the discussion of EOL decisions with the patient's family and other health care workers, and the reasons given for the lack of discussions with families. Differences may also be related to variations in physician self-reporting. None of the religions evaluated in this study allow active euthanasia or SDP, but they allow withholding life-sustaining therapies [22–29].
The Catholic Church allows withdrawing of futile therapy and alleviation of pain and suffering in the dying with life shortening as a nonintended side effect (see “Evangelium Vitae”, 25 March 1995, Sect. 65, http://www.newadvent.org/library/docs_jp02ev.htm; “A Catechismus Catholicae Ecclesiae”, 1997, Sects. 2278, 2279). The majority of Protestant churches accept withholding and withdrawing treatments if found appropriate by the treating physician [24], but controversies do exist [22]. The Greek Orthodox church is adamant in rejecting intentional shortening of life by withdrawing therapy [25]. Although 96% of Greek Orthodox believe that communication is important in the final stage of a disease, only 23% agree that the patient should be informed of the prognosis [26]. Jewish law or Halacha, also does notallow withdrawing of life-sustaining treatments because human life is of infinite value and the hastening of death even in the terminally ill is not allowed [27, 28] According to Islamic bioethics, withholding and withdrawing treatment is allowed in the terminally ill, but the intention must never be to hasten death, only to abstain from overzealous treatment [29].
In this study Catholics (both patients and physicians) formed the largest group. Although the smallest group was Moslem, accounting for fewer than 1% of the physicians and patients, which calls for caution in the interpretation of results for this religion, little is known about EOL practices in this culture [30], and therefore these results add important information. Interestingly, a large number of physicians, 22%, identified themselves as having no religious affiliation.
As the Christian and Islamic religions allow withdrawal of therapy, Catholic, Protestant, and Moslem physicians had higher rates of withdrawal (53%, 49%, and 37%, respectively) rather than Jewish (19%) and Greek Orthodox (22%) physicians, whose religion does not allow withdrawal. No Jewish or Greek Orthodox physician performed SDP. The Catholic rate of withdrawal here (53%) is much higher than in prior studies on Catholics answering hypothetical questions [1, 2]. A Spanish study (where physicians were presumably Catholic) also found a much higher rate of withdrawing than withholding therapy [31]. That Protestant physicians were likely to withdraw life-sustaining therapy is consistent with a previous study [1].
The rate of withdrawing treatment (37%) among Moslem physicians in this study was higher than recent studies from Lebanon (14%) and Turkey (9%) [11, 32]. This may be related to the Lebanese and Turkish physicians' belief that withdrawing treatment is intented to hasten death and is therefore prohibited. As with the Catholic physicians, the actions of Greek Orthodox and Jewish physicians may be related to cultural factors in addition to religion as most were from the Southern region. Greek Orthodox had the longest time until limitations of all groups of patients. This may be related to the more conservative Greek Orthodox patients or families requesting more treatments and fewer limitations [3, 9].
The relatively low percentage of therapy withdrawal (especially ventilators) in the present study for Jewish physicians can be explained by Jewish law not allowing the hastening of death [26, 27]. A possible cultural influence is seen, since Jewish physicians withdrew in 36% instances in the North vs. only 6% in the South. Previous investigations, however, revealed regional differences among Jewish physicians. In one study [2] Jewish physicians in Pennsylvania, USA, were relatively less willing to withdraw life support, while in another study North American Jewish health care providers were more willing to limit therapy [33]. These data show that although the impact of religion on treatment decisions is important, it may at least in part be lost with acculturation.
At the time of this study euthanasia was illegal in all European countries, although legally pardoned in The Netherlands. That Catholic and Protestant physicians were willing to perform SDP despite their religion's disapproval of this practice probably reflects the complexity of the various factors affecting' decisions, causing physicians belonging to the same religion to act differently in different countries. It also reflects the strong impact of regional culture as most cases took place in the more liberal Central and Northern countries while only one case took place in the conservative South [3, 9] which is similar to findings that physicians change attitudes and practices when they move to a different culture [12, 13]. It is also possible that Catholic physicians did not view their actions as intentional life ending actions but rather as alleviation of suffering in the dying with life shortening as a nonintended side effect which is permissible (“Evangelium Vitae”, 25 March 1995, Sect. 65, http://www.newadvent.org/library/docs_jp02ev.htm; “A Catechismus Catholicae Ecclesiae”, 1997, Sects. 2278, 2279). Information about EOL wishes was available for only one-quarter of the patients, highest among patients whose physician was Protestant. This is probably due to greater respect for patient autonomy in the North, while the relatively low numbers for Catholic physicians might reflect more paternalistic attitudes of the South. In approximately one-third of the cases EOL decisions were not discussed with family members, and there were differences based on religious affiliation.
Greater religiosity correlates with more prolonged care and reluctance to withdraw life-sustaining therapy [5–7]. Neonatologists rating religion as extremely or fairly important were less likely to withhold or withdraw intensive treatments [5]. In another neonatologist study nonreligious respondents had a stronger quality-of-life attitude than religious respondents, but the effects of religiosity were statistically nonsignificant once pro-life vs. quality-of-life attitudes were included in the model [6]. This suggests that religion may have been one of several factors affecting physician attitudes to therapy. This study did not examine the degree of physician religiosity, but it was able to compare physicians with no religious affiliation to physicians having different religious affiliations. There were differences in EOL practices between physicians affiliated with a religion and those who were not. Decisions did not move in the same direction, indicating the complex interaction between culture and religious affiliation. Although religious affiliation is important, the strong cultural influence is apparent with greater withdrawing occurring for physicians with and without religions in the North than in the South. It is recognized that physician practices are based on local legal and moral constraints in addition to religious beliefs and many physicians or patients may not follow their religion's doctrines.
Results of the present multivariate analysis showed no relationship between the presence of chronic disorders and withdrawal decisions as opposed to the previous Ethicus report [3]. This is probably due to the fact that the original report looked at the odds of any limitation vs. CPR whereas the present study evaluated the odds of withdrawing vs. withholding therapy.
Strengths of the present study are its being the first large prospective study of consecutive patients assessing the impact of different religious affiliations on ICU EOL practices and evaluation of physicians' actual practice rather than responses to a hypothetical questionnaire. The present study, however, has limitations. Since only one to four centers (with physicians with special interest in ethical issues) participated in each country, these centers may not necessarily be representative of all ICUs in that country. The religious affiliation of many patients was unknown because the waiver of informed consent required no interventions (asking patient's religion) as part of the study. There was more information for religious affiliation but paucity about cultural information; the latter caused difficulty in drawing general conclusions from relatively limited data. Other associated factors not measured in the study may have a major influence on the results including degree of religiosity, family religious affiliation, social traditions, local regulations and laws. Underreporting of practices for fear of legal ramifications cannot be excluded.
The significant differences in ICU practices between physicians of different religious affiliations and cultures highlight the importance of religion and culture on medical practice at the EOL. Understanding the religious influences on EOL choices may explain conflicts and assist in developing a consensus and guidelines for EOL practices. There is also a need for a better understanding of patient and family religious concerns at the EOL, particularly as patients and families of certain religions may consider withdrawal of life-sustaining therapies as homicide. Decisions that run contrary to patients' strongly held religious or personal beliefs which are made without the patients' or surrogates' knowledge or discussion represent a serious ethical problem in end-of-life ICU care.
References
Vincent JL (1999) Forgoing life support in western European intensive care units: the results of an ethical questionnaire. Crit Care Med 27:1626–1633
Christakis NA, Asch DA (1995) Physician characteristics associated with decisions to withdraw life support. Am J Public Health 85:367–372
Sprung CL, Cohen SL, Sjokvist P, Baras M, Bülow HH, Hovilehto S, Ledoux D, Lippert A, Maia P, Phelan D, Schobersberger W, Wennberg E, Woodcock T (2003) End-of-life practices in European intensive care units. The Ethicus study. JAMA 290:790–797
Richter J, Eisenmann M, Zgonnika E (2001) Doctors' authoritarianism in end of life treatment decisions. A comparison between Russia, Sweden and Germany. J Med Ethics 27:186–191
Cuttini M, Nadai M, Kaminski M, Hansen G, de Leeuw R, Lenoir S, Persson J, Rabagliato M, Reid M, de Vonderweid U, Lenard HG, Orzalesi M, Saracci R (2000) End-of-life decisions in neonatal intensive care: physicians' self-reported practices in seven European countries. Lancet 355:2112–2118
Rebagliato M, Cuttini M, Broggin L, Berbik I, de Vonderweid U, Hansen G, Kaminski M, Kollee LA, Kucinskas A, Lenoir S, Levin A, Persson J, Reid M, Saracci R (2000) Neonatal end-of-life decision making. Physicians attitudes and relationship with self-reported practices in 10 European countries. JAMA 284:2451–2459
Willems DL, Daniels ER, van der Wal G, van der Maas PJ, Emanuel EJ (2000) Attitudes and practices concerning the end of life. Arch Intern Med 160:63–68
Alemayehu E, Molloy DW, Guyatt GH, Singer J, Penington G, Basile J, Eisemann M, Finucane P, McMurdo ME, Powell C (1991) Variability in physicians' decisions on caring for chronically ill elderly patients: an international study. Can Med Assoc J 144:1133–1138
Cohen S, Sprung CL, Sjokvist P, Lippert A, Ricou B, Baras M, Hovilehto S, Maia P, Phelan D, Reinhart K, Werdan K, Bülow HH, Woodcock T (2005) Communication of end of life decisions in European intensive care units. Intensive Care Med 31:1215–1221
Yaguchi A, Truog RD, Curtiss JR, Luce JM, Levy MM, Melot C, Vincent JL (2005) International differences in end-of-life attitudes in the intensive care unit. Arch Intern Med 165:1970–1975
Yazigi A, Riachi M, Dabbar G (2005) Withholding and withdrawal of life-sustaining treatment in a Lebanese intensive care unit: a prospective observational study. Intensive Care Med 31:562–567
Matsumura S, Bito S, Liu H, Kahn K, Eukuhara S, Kagawa-Singer M, Wenger N (2002) Acculturation of attitudes toward end-of-life care. J Gen Intern Med 17:531–539
Asai A, Fukuhara S, Lo B (1995) Attitudes of Japanese and Japanese-American physicians towards life-sustaining treatment. Lancet 346:356–359
Cook D, Guyatt GH, Jaeschke R, Reeve J, Spanier A, King D, Molloy DW, Willan A, Streiner DL (1995) Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill. JAMA 273:703–707
Prendergast TJ, Claessens MT, Luce JM (1998) A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med 158:1163–1167
Task Force on Ethics of the Society of Critical Care Medicine (1990) Consensus statement on the ethics of foregoing life-sustaining treatments in the critically ill. Crit Care Med 18:1435–1439
Lanken PN, Ahlheit BD, Crawford S, Hansen-Flaschen JH, Lefrak SS, Luce JM, Matthay MA, Osborne ML, Raffin TA, Robotham JL, Selecky PA, Snider GL, Storey DD, Terry PB, Cohen CB, Jonsen AR, Meisel A, Nelson LJ, Weiss EC (1991) Withholding and withdrawing life-sustaining therapy. Am Rev Respir Dis 144:726–731
SUPPORT Principal Investigators (1995) A controlled trial to improve care for seriously ill hospitalized patients. JAMA 274:1591–1598
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, Mcintyre L, Tulsky JA (2000) Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482
Cardoso T, Fonseca T, Pereira S, Lencastre L (2003) Life-sustaining treatment decisions in Portuguese intensive care units: a national survey of intensive care physicians. Crit Care 7:167–175
Sprung CL, Maia P, Bulow HH, Ricou B, Armaganidis A, Baras M, Wennberg E, Reinhart K, Cohen SL, Fries DR, Nakos G, Thijs LG (2005) Presented in part at the 18th Annual Congress European Society of Intensive Care Medicine, Amsterdam
Engelhardt HT, Iltis AS (2005) End-of-life: The traditional Christian view. Lancet 366:1045–1049
Magnusson MA (2004) The new Protestants. Reluctance towards European integration in northern Europe. Research paper series no 1. Bifröst School of Business, Iceland; http://www.bifrost.is/files/skra_0007517.pdf
Pauls M, Hutchinson RC (2002) Bioethics for clinicians. Protestant bioethics. CJAM 166:339–343
Hatzinikolaou N (2003) Prolonging life or hindering death? An Orthodox perspective on death, dying and euthanasia. Christian Bioethics 9:187–201
Mystakidou K, Parpa E, Tsilika E, Katsouda E, Vlahos L (2005) The evolution of euthanasia and its perceptions in Greek culture and civilization. Perspect Biol Med 48:95–104
Rosner F, Tendler MD (1980) Euthanasia. In: Rosner F, Tendler MD (eds) Practical medical halacha. Feldheim Jerusalem, p 56
Steinberg A, Sprung CL (2006) The dying patient: new Israeli legislation. Intensive Care Med 32:1234–1237
Ebrahim AFM (2000) The living will (Wasiyat Al-Hayy): a study of its legality in the light of Islamic jurisprudence. Med Law 19:147–160
Pochard F, Abroug F (2005) End-of-life decisions in ICU and cultural specifities. Intensive Care Med 31:506–507
Esteban A, Gordo F, Solsona JF, Alia I, Caballero J, Bouza C, Alcala-Zamora J, Cook DJ, Sanchez JM, Abizanda R, Miro G, Fernandez Del Cabo MJ, de Miguel E, Santos JA, Balerdi B (2001) Withdrawing and withholding life support in the intensive care unit: a Spanish multicentre study. Intensive Care Med 27:1744–1749
Iyilikci L, Erbayraktar S, Gökmen N, Ellidokuz H, Kara HC, Gunerli A (2004) Practices of anaesthesiologists with regard to withholding and withdrawal of life support from the critically ill in Turkey. Acta Anaesth Scand 48:457–462
Society of Critical Care Medicine Ethics Committee (1992) Attitudes of critical care medicine professionals concerning forgoing life-sustaining treatments. Crit Care Med 20:320–326
Acknowledgements
This study was funded as part of the European Concerted Action project Ethicus – “End of Life Decision Making and Life Ending Procedures in European Intensive Care Units” funded by the European Commission (contract no. PL 963733), in part by grant no. 4226 from the Chief Scientist's Office of the Ministry of Health, Israel, in part by OFES Switzerland (Biomed) no. 980271, in part by the European Society of Intensive Care Medicine and in part by the Walter F. and Alice Gorham Foundation, Inc. The authors are solely responsible for the publication, it does not represent the opinion of the European Commission, and the Commission is not responsible for any use of the published data.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00134-007-0781-1
Rights and permissions
About this article
Cite this article
Sprung, C.L., Maia, P., Bulow, HH. et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med 33, 1732–1739 (2007). https://doi.org/10.1007/s00134-007-0693-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0693-0