Abstract
Objective
To obtain insight into the occurrence of brain death and the potential for brain dead and controlled non-heart-beating organ donors (CNHB) in patients with traumatic brain injury (TBI), subarachnoid haemorrhage (SAH) and intracerebral haemorrhage (ICH) in a large neurosurgical serving area (2.1 million inhabitants).
Design
Retrospective analysis of data concerning patients with TBI, SAH and ICH who died during the course of ICU treatment during 1999–2003.
Setting
A 16-bed neuro-intensive care unit.
Patients
Patients with TBI, SAH or ICH who died during the course of ICU treatment.
Measurements and results
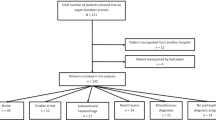
The number of ICU deaths in patients with TBI, SAH and ICH declined from 111 in 1999 to 64 in 2003. In total, 476 deaths occurred. Of these, 177 patients were not included in the analysis. Two hundred ninety-nine (299) ventilated patients had two or more absent brainstem reflexes (ABSR) and a Glasgow Coma Score of 3–4 at the moment of treatment withdrawal and formed the potential for organ donation; 61 of these patients were treated until full brain death. Organs of 57 patients could be harvested. We analysed the reasons that organs were not procured in the 242 remaining patients. The most important reasons were family refusal (32%), medical contraindications (14%), and the treating physician not considering potential organ donation (20%). The missed potential is 162/299 (54%).
Conclusions
The number of actual and potential organ donors is declining, but a considerable number of potential CNHB donors exists. Refusal by relatives is the most important reason for failure to procure organs.
Similar content being viewed by others
References
Pugliese MR, Esposti DD, Dormi A, Venturoli N, Gaito PM, Buscaroli A, Petropulacos K, Costa AN, Ridolfi L (2003) Improving donor identification with the donor action programme. Trans Int 16:21–25
Sprung CL, Cohen SL, Sjokvist P, Baras M, Bulow HH, Hovilehto S, Ledoux D, Lippert A, Maia P, Phelan D, Schobersberger W, Wennberg E, Woodcock T (2004) End-of-life practices in European intensive care units. JAMA 290:790–797
Navarro A (1996) Brain death epidemiology; the Madrid study. Transplant Proc 28:103–104
Salih MAM, Harvey I, Frankel S, Coupe DJ, Webb M, Cripps HA (1991) Potential availability of cadaver organs for transplantation. BMJ 302:1053–1055
Chiara O, Scott JD, Cimbanassi S, Marini A, Zoia R, Rodriguez A, Scalea T, Colombo F, Freni L, Padalino P, Segala M, Tiberio G, Giovanola M, Pellegrinelli M, Macrì L, Omboni E, Iapichino G, Baticci F, Cerchiari E, Guffanti E, Pugliese R, Sesana G, Martinetti R, Ronchi E, Staudacher C, Carlucci M, Sotttili S, Trevano GQ (2002) Trauma deaths in an Italian urban area: an audit of pre-hospital and in-hospital trauma care. Injury 33:553–562
Senouci K, Guerrini P, Diene E, Atinault A, Claquin J, Bonnet F, Tuppin P (2004) A survey on patients admitted in severe coma: implications for brain death identification and organ donation. Intensive Care Med 30:38–44
Altinörs N, Benli S, Caner H, Altaş A, Bavbek M, Bilgin N (1998) Brain dead donors for organ transplantation. Transplant Proc 30:771–772
Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ (2002) Specialist neurocritical care and outcome from head injury. Intensive Care Med 28:547–553
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A (1994) Initial and recurrent bleeding are the major causes of death following subarachnoid haemorrhage. Stroke 25:1342–1347
Dominguez-Roldan JM, Garcia-Alfaro C, Diaz-Parejo P, Barrera-Chacon JM, Caldera-Gonzalez A, Murillo-Cabezas F (2002) Identification of subarachnoid hemorrhages with high risk of evolution to brain death. Transplant Proc 34:9–10
Dşemeci L, Yilmaz M, Cengiz M, Dora B, Ramazanoðlu A (2004) Brain death and donor management in the intensive care unit: experiences over the last 3 years. Transplant Proc 36:20–21
Pratschke J, Paz D, Wilhelm MJ, Laskowski I, Kofla G, Vergopoulos A, MacKenzie HJ, Tullius S, Neuhaus P, Hancock WW, Volk HD, Tilney NL (2004) Donor hypertension increases graft immunogenicity and increases chronic changes in long-standing renal allografts. Transplantation 77:43–48
Morris PJ, Johnsonm RJ, Fuggle SV, Belger MA, Briggs JD (1999) Analysis of factors that affect outcome of primary cadaveric renal transplantation in the UK. Lancet 354:1147–1152
Tullius SG, Volk HD, Neuhaus P (2001) Transplantation of organs from marginal donors. Transplantation 72:1341–1349
Dominguez-Roldan JM, Barrera-Chacon JM, Martin-Bermudez R, Santamaria-Milsut JL, Flores-Cordero JM, Gonzalez PJ (1999) High-risk spontaneous cerebral hematomas leading to brain death: early detection of potential organ donors. Transplant Proc 31:2595–2596
Schaeffer MJ, Johnson E, Suddaby EC, Suddaby SC, Brigman LE (1998) Analysis of donor versus nondonor demographics. J Transpl Coord 8:9–15
Siminoff LA, Gordon N, Hewlett J, Arnold RM (2001) Factors influencing families consent for donation of solid organs for transplantation. JAMA 286:71–77
Matesanz R, Miranda B (2002) A decade of continuous improvement in cadaveric organ donation: The Spanish model. J Nephrol 15:22–22
Procaccio F, Barbacini S, Meroni M, Sarpellon M, Verlato R, Giron GP (2001) Deaths with acute cerebral lesion and heart-beating potential organ donors in the Veneto Region. Minerva Anestesiol 67:71–78
Opdam HI, Silvester W (2004) Identifying the potential organ donor: an audit of hospital deaths. Intensive Care Med 20:1390–1397
Kleindienst A, Haupt WF, Hildebrandt G (1999) Brain death and organ donation in Germany: analysis of procurement in a neurosurgical unit and review of press reports. Acta Neurochir (Wien) 141:641–646
Faltin DL, Jeannet M, Suter PM (1992) The decrease in organ donations from 1985 to 1990 caused by increasing medical contraindications and refusals by relatives. Transplantation 54:85–88
Gore SM, Hinds CJ, Rutherford AJ (1989) Organ donation from intensive care units in England. BMJ 299:1193–1197
Sheehy E, Conrad SL, Brigham LE, Luskin R, Weber P, Eakin M, Schkade L, Hunsicker L (2003) Estimating the number of potential organ donors in the United States. N Engl J Med 349:667–674
Cohen B, Smits JM, Haase B, Persijn G, Vanrenterghem Y, Frei U (2005) Expanding the donor pool to increase renal transplantation. Nephrol Dial Transplan 20:34–41
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kompanje, E.J.O., Bakker, J., Slieker, F.J.A. et al. Organ donations and unused potential donations in traumatic brain injury, subarachnoid haemorrhage and intracerebral haemorrhage. Intensive Care Med 32, 217–222 (2006). https://doi.org/10.1007/s00134-005-0001-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0001-9